If you’re dealing with severe back pain, you’ve probably heard terms like “bulging disc” or “herniated disc” thrown around. While these conditions sound similar and are often used interchangeably, they actually describe two distinct problems that require different treatment approaches. If you’ve been diagnosed with either condition or suspect you might have disc problems, understanding the difference is the first step toward effective relief.
The pain from disc problems can be more than just an inconvenience. It can make sleeping impossible, turn simple tasks like tying your shoes into major challenges, and steal away the activities you love. The good news? Understanding what’s actually happening in your spine puts you on the path to real solutions.
The Anatomy of Your Spinal Discs
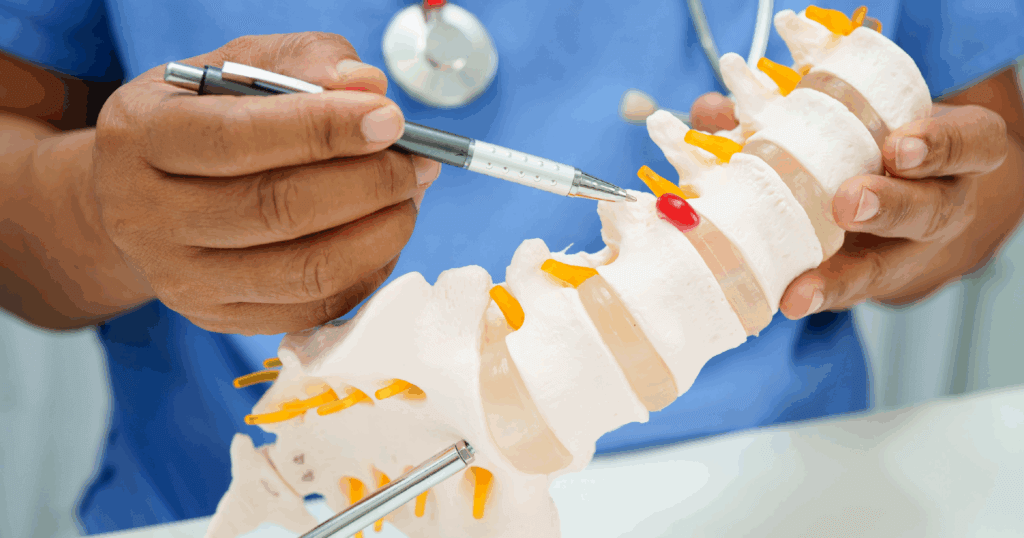
Before we dive into the differences, let’s talk about what spinal discs actually are. Your spine contains 24 vertebrae stacked on top of each other, and between each of these bones sits a cushion-like disc. These discs are incredibly important because they act as shock absorbers for your spine, allowing you to bend, twist, and move through your daily activities without bone-on-bone grinding.
Each disc has two main parts: the tough outer layer called the annulus fibrosis and the soft, gel-like inner core called the nucleus pulposus. Think of it like a jelly donut, with a firm outer shell protecting the softer filling inside. When these discs are healthy, they keep your spine flexible and protected. When they’re damaged, that’s when problems start.
What Is a Bulging Disc?
A bulging disc occurs when the outer layer of the disc extends beyond its normal position in the spinal column. The disc essentially bulges outward, but the tough outer layer remains intact. This is a relatively common condition and can happen naturally as part of the aging process.
With a bulging disc, the entire disc protrudes outward. The key point here is that while the disc has moved out of its normal position, there’s no tear or rupture in the outer layer. The gel-like center remains safely contained within the disc.
Many people with bulging discs don’t even know they have them. Medical imaging studies have shown that a significant number of people over 40 have bulging discs without experiencing any symptoms at all. However, when a bulging disc presses on nearby nerves, it can cause:
- Dull or aching pain in the affected area
- Muscle weakness
- Tingling or numbness if the bulge presses on a nerve
- Discomfort that worsens with certain movements
Bulging discs typically develop gradually over time due to natural aging, repetitive movements, poor posture habits, or degenerative changes. The disc slowly changes shape as the outer layer weakens, but it remains structurally intact.
What Is a Herniated Disc?
A herniated disc is a more severe condition where the outer layer of the disc actually tears or ruptures, allowing the soft inner material to push through. This is sometimes called a ruptured disc or slipped disc, though the disc doesn’t actually slip out of place.
When the inner gel-like material escapes through the tear, it can press directly on nearby nerves, causing more intense pain and symptoms than a bulging disc typically would. The herniated material can also trigger an inflammatory response in the surrounding tissues, adding to the discomfort.
Herniated disc symptoms are often more severe and noticeable:
- Sharp, shooting pain that radiates down the leg (sciatica) or arm
- Significant numbness or tingling
- Muscle cramping or spasms
- Weakness in the affected limb
- Difficulty with certain movements
- In severe cases, loss of bladder or bowel control (this is a medical emergency)
A herniated disc can occur suddenly from trauma such as a car accident or improper lifting. It can also be the result of a bulging disc that has progressively worsened over time, where the weakened outer layer eventually tears under stress.
The Key Differences
The main difference between bulging and herniated discs comes down to the integrity of the outer layer:
Bulging Disc: The outer layer remains intact, but the entire disc extends beyond its normal boundaries. Think of it as the disc changing shape but staying in one piece.
Herniated Disc: The outer layer has torn or ruptured, allowing the inner material to escape. This is a more serious structural problem that often causes more severe symptoms.
Another important distinction is severity and development. Bulging discs usually develop slowly over time as part of natural degeneration. Herniated discs can develop suddenly from an injury or can be the final stage of a progressively weakening bulging disc.
The symptoms also tend to differ in intensity. While bulging discs can certainly cause discomfort, they may produce no symptoms at all or only mild pain. Herniated discs more commonly produce sharp, intense pain along with numbness, tingling, or weakness that radiates down the arms or legs because the herniated material is more likely to directly compress nerve roots.
How Location Affects Your Symptoms
Where your disc problem occurs in the spine makes a big difference in the symptoms you experience. Most disc problems happen in the lower back (lumbar spine) or the neck (cervical spine), as these areas move the most and bear the most stress.
Lumbar Spine (Lower Back): Disc problems here often cause lower back pain that may radiate into the buttocks, hips, legs, and feet. This is commonly known as sciatica when the pain travels down the leg.
Cervical Spine (Neck): Disc issues in the neck can cause pain, numbness, or weakness in the shoulders, arms, and hands. You might also experience headaches or neck stiffness. Neck adjustment may be part of your treatment plan for cervical disc problems.
Treatment Options: Effective Relief Without Surgery
The most encouraging news for those suffering from either condition is that surgery is rarely your first or only option. At Carlson Chiropractic Center, we’ve helped countless patients find relief through comprehensive, conservative care focused on whole-body health and wellness.
Spinal Decompression Therapy
Spinal decompression therapy has been clinically proven effective for pain associated with both herniated and bulging discs. This safe, drug-free, non-surgical approach uses computerized traction to gently stretch the spine, creating negative pressure within the disc.
This vacuum effect can:
- Pull the herniated or bulging disc material back toward its proper position
- Reduce pressure on compressed nerves
- Increase blood flow and nutrient delivery to the damaged disc
- Promote natural healing without surgery
- Provide effective lower back pain relief and pinched nerve relief
Research backs up what we see in practice. Studies have documented the reduction of disc herniations, confirmed by MRI imaging, in the majority of patients treated with spinal decompression therapy. Another study found that the majority of patients with ruptured discs achieved good to excellent results after completing treatment.
At Carlson Chiropractic Center, we use the Kennedy Decompression system. “We chose the Kennedy Decompression system after a significant amount of research,” Dr. Carlson explains. “With its unparalleled design and proven history, the Kennedy system is the ‘gold standard’ in decompressive therapy. We also selected this system because it can treat discs in the neck and low back.”
The treatment promotes the movement of oxygen, water, and nutrient-rich fluids into the spinal discs, giving them the environment they need to heal properly.
Chiropractic Care
Regular chiropractic care helps restore proper spinal alignment and mobility, which takes stress off injured discs and supports recovery. Our chiropractic doctors combine spinal adjustments with other therapies to address the underlying causes and prevent future problems. The benefits of chiropractic care extend beyond pain relief to support overall chiropractic health and wellness.
Complementary Therapies
We often combine spinal decompression and chiropractic adjustments with:
- Ice and heat therapy
- Electrical stimulation
- Lifestyle and postural modifications
- Ergonomic recommendations for work and home
Most patients with either condition can avoid surgery through committed conservative care as part of a comprehensive wellness plan. The key is early treatment. The longer you live with an untreated disc problem, the more difficult it can become to resolve.
When to Seek Professional Help
If you’re experiencing persistent back pain or neck pain, it’s time to get evaluated. Don’t wait until the pain becomes unbearable or starts seriously impacting your daily life. Both bulging and herniated discs respond better to treatment when they’re addressed promptly. Instead of a walk-in clinic, give us a call to secure your spot!
You should seek professional evaluation if you experience:
- Persistent back or neck pain lasting more than a few days
- Pain that radiates down your arms or legs
- Numbness, tingling, or weakness in your extremities
- Pain that worsens over time rather than improving
- Difficulty with balance or coordination
- Loss of bladder or bowel control (this is a medical emergency)
We conduct thorough examinations and review imaging studies like MRIs to accurately diagnose disc problems. If you’re searching for a “chiropractor near me” or “spinal decompression therapy near me”?, we’re here to help. Discover how we can help you find the relief you’ve been searching for.